- Foundation
- Actions
- Osteoarthritis
- Osteoporosis
- Actuality
- OAFI Radio/TV
- Get Involved
- Contact
-
-
-
OAFI
Osteoarthritis International FoundationC/ Tuset, 19 · 3º 2ª
08006 Barcelona
(+34) 931 594 015
info@oafifoundation.comSchedule:
Monday-Thursday 9AM-6PM
Friday 8AM-3PM
-
-
-

-

-

Gestation and Lactation: Sustainable Bone Health

During pregnancy and lactation, the mother’s bone health may deteriorate, increasing the risk of fractures and permanent sequelae.
Article published by Sandra Toril Coca and Jose Luis Baquero, Marina Baquero, Nina Martínez and Josep Vergés in New Medical Economics.
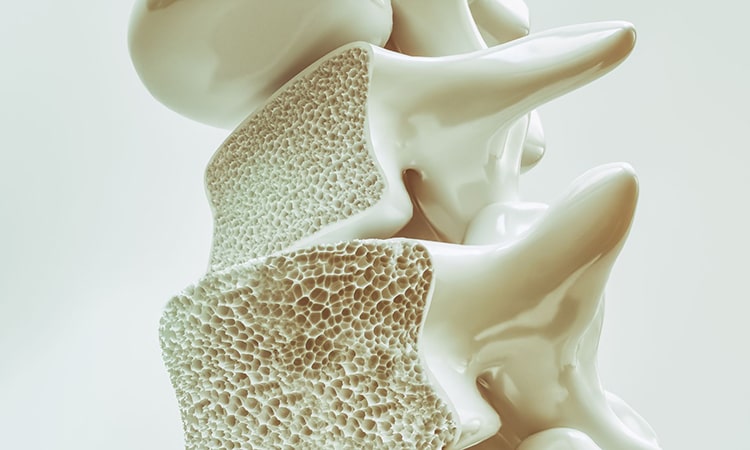
Osteoporosis during pregnancy and breastfeeding
Osteoporosis during pregnancy and lactation, although rare, it can occur and cause bone fractures, especially in areas such as the spine, pelvis and hip. This phenomenon is known as transient osteoporosis of pregnancy, and later as osteoporosis associated with lactation.
During both periods, calcium requirements increase considerably, for the development of the foetus and for the production of maternal milk. In fact, the foetus needs approximately 30 grams of calcium during gestation (80% in the third trimester); and during lactation, the mother loses 200-300 mg of calcium per day through the milk.
To compensate for this loss, certain changes occur in the mother, such as an increase in the intestinal absorption of calcium (mainly mediated by vitamin D), a decrease in renal excretion, and an increase in bone resorption of the maternal skeleton itself. This last mechanism can lead to osteopenia and even osteoporosis if there are nutritional deficiencies, hormonal alterations, genetic predisposition or concomitant treatments, among other factors.
Let us not forget that the course of the disease is silent, with no apparent symptoms, but that the risk of fragility fracture is increased twice as much in the osteopenia stage and four times as much in the osteoporosis stage.
The Process
In most cases, bone loss is temporary and reversible; and when breastfeeding is discontinued and normal hormone levels are restored, the body re-establishes the physiological mechanisms that restore mineral density and bone functionality. However, in some women, fragility fractures occur, particularly in the vertebrae and pelvis, especially in the third trimester of pregnancy and/or the first months after childbirth. These fractures are associated with sudden back pain and/or functional limitation, severely affecting the mother’s quality of life and may become permanent.
The Diagnosis
Diagnosis of maternal osteoporosis is challenging. DEXA bone densitometry is not recommended during pregnancy due to radiation exposure with risk to the foetus. However, there are safe alternatives to assess bone health, such as bone ultrasound using portable devices that measure bone density without radiation, in the foot (validated Calcaneal Ultrasonic Densitometry test – UCD) or in other anatomical areas; as well as analysis of calcium, vitamin D and other markers, along with a detailed clinical evaluation and family and personal history. In this evaluation it is essential to assess risk factors: sedentary lifestyle, osteopenizante treatments (such as corticosteroids and heparin), certain previous or concomitant pathologies such as diabetes, oncology, hyperthyroidism, intestinal malabsorption, or celiac disease; to guide early diagnosis and early intervention.
In addition, there are instruments for calculating the risk of suffering a fracture, such as the FRAX® tool (Fracture Risk Assessment Tool), developed by the World Health Organisation, to estimate the risk of fracture at 10 years, even in the absence of densitometry, assessing clinical factors such as age, body mass index (based on weight and height), history of fractures and family history, use of glucocorticoids, arthritis, tobacco and alcohol consumption, among others. Although it is validated from the age of 40 onwards, it can be useful as an orientative tool in young women, assuming its limitations.
Nutrition during pregnancy and lactation
The mother’s nutrition must address the quantity, but also the quality of nutrients. In addition to calcium, several minerals are essential for bone health, such as phosphorus, magnesium, zinc, copper, manganese, boron and selenium, for their role in bone mineralisation; as well as potassium, fluoride and iron, which have an indirect role in the synthesis of the organic or structural matrix. Vitamins D and K contribute to mineralisation, while vitamins C and B vitamins support the formation of collagen, a key component of bone and joints.
In bone health in pregnancy and lactation, as important as adequate mineralisation is the integrity of the three-dimensional structure of collagen fibres, which represents about 90% of the organic matrix of bone. This collagen network supports hydroxyapatite crystals (formed by calcium and phosphate), and is responsible for essential mechanical characteristics such as flexibility, elasticity and tensile strength, among others.

Physical activity during pregnancy and lactation
It is also important to highlight that adapted physical activity during pregnancy and breastfeeding, under professional supervision, can help maintain bone density, improve postural balance and prevent falls, thus reducing the risk of fracture. Likewise, the promotion of exercise during adolescence and young adulthood, before motherhood, is key in the formation of optimal bone mass to protect later in life.
For this reason a multidisciplinary and preventive approach is required, starting with education from an early age, encouraging self-care and the practice of healthy habits such as regular physical activity, adequate nutrition, moderate sun exposure, and avoiding smoking and alcohol. It is essential to ensure optimal levels of calcium and vitamin D among others (assessing the need for supplementation of these elements, collagen, etc.), control pain if symptoms are already present, and even consider the temporary suspension of breastfeeding. Subsequently, some patients may require pharmacological treatment with antiresorptive or bone-forming drugs (contraindicated during pregnancy and lactation), as well as therapies to treat secondary causes such as hyperparathyroidism or hypovitaminosis D; and even in certain cases, it will be necessary to assess surgical interventions and individualised functional rehabilitation plans.
However, maternity-related osteoporosis often results from a multifactorial combination of causes, and remains an under-researched and under-attended condition. Its true incidence is still unknown, despite the serious consequences it can have for the mother. More studies of prevalence, triggers, risk profiles, efficacy of interventions and patient experience are needed.
While parameters such as iron and folic acid are routinely monitored in pregnancy, how many women receive a risk assessment for osteoporosis and fragility fracture, and how many undergo a simple vitamin D and calcium test (which requires a simple finger prick)?
Are symptoms underestimated?
In many cases, the symptoms of maternal osteoporosis during pregnancy and lactation are underestimated or mistakenly associated with other musculoskeletal disorders and even psychological causes, which delays both diagnosis and management. As a consequence, many mothers find their postpartum recovery compromised, experience disabling pain that prevents them from caring for their newborn or self-care, and in more severe cases, develop chronic pain and functional disability.
As we have seen, the consequences can be severe: persistent pain due to microfractures, difficulty carrying weight or moving normally, impaired quality of life, increased risk of further fractures if bone loss is not detected and treated, and significant emotional repercussions as the stress of motherhood overlaps with physical pain and dependency.
Solutions
For all these reasons, education, prevention and early diagnosis during pregnancy and breastfeeding are of paramount importance, integrating them from the very preparation for childbirth. Raising the awareness of healthcare personnel, specific training in perinatal bone health and the development of adapted clinical protocols are key to progress in this direction. It is necessary that monitoring guidelines and protocols incorporate this assessment, to prevent an avoidable condition from leading to disabling consequences for young women at such a critical time in their lives.
In OAFI, we continue to work to improve the approach, visibility and quality of life of all people suffering from osteoarticular pathologies, many of them young women of childbearing age.
You can contact us in Barcelona, c/ Tuset, 19- 3º 2ª, by phone at 931 594 015 or by email at info@oafifoundation.com.
Article published by Sandra Toril Coca and Jose Luis Baquero, Marina Baquero, Nina Martínez and Josep Vergés in New Medical Economics.