- Foundation
- Actions
- Osteoarthritis
- Actuality
- OAFI Radio/TV
- Get Involved
- Contact
-
-
-
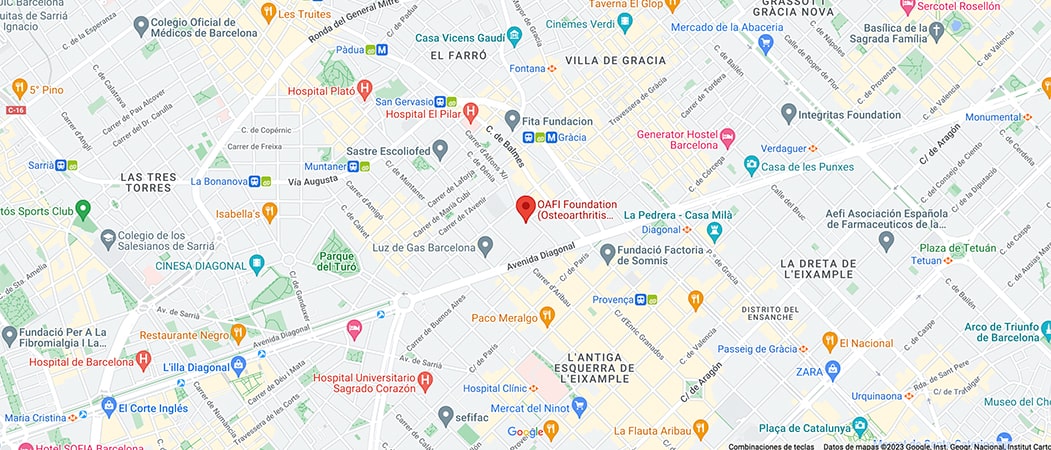
OAFI
Osteoarthritis International FoundationC/ Tuset, 19 · 3º 2ª
08006 Barcelona
(+34) 931 594 015
info@oafifoundation.comSchedule:
Monday-Thursday 9AM-6PM
Friday 8AM-3PM
-
-
-

-

-

Socio-health care model

- On May 8th, was held “Adefarma Work”, event that included round tables on different current issues in the health and social-health sector.
- The round table: “WHAT IS THE DEPENDENCY SERVICE THAT COMMUNITY PHARMACY PHARMACY PROVIDES? POTENTIAL, RISKS, THREATS, STRENGTHS” had the participation of the following speakers Dª Ana Oliver, Vicepresidenta del grupo Hefame, Dª. Nuria Urquiz Pérez, Directora del Centro sociosanitario L´ Onada, Onacare, Dra. Alexandra Gonzalez Pinto Departamento médico L´ Onada, Onacare, Dr. José Luis Baquero Úbeda, patient and CSR, IR and access coordinator in OAFI, and Secretary at AECOSAR and Dr. Rubén Martín Lázaro, secretario General de Adefarma.
- It had the explicit support of representatives of the industry through Mr. Francisco Javier Labarga, Business Unit Manager at Tecnimede España.
- There was unanimous agreement on how the pharmaceutical service should be provided to social and healthcare centers; as needed by the patient, each one of them. Flexible, competitive, immediate and, above all, it should revolve around the freedom of choice of the centers and patients, regardless of where the center is located, the number of residents and their regimen.
Socio-health care model
Recently, in the professional world of community pharmacy, in the centers and patient associations, there has been quite a stir in the Community of Madrid. Due to the fact that the General Directorate of Social and Health Coordination of the CAM’s Health Department has reportedly stated its interpretation of what is contained in the Autonomous Management Law on the development of pharmaceutical services in residential Social Services Centers, linking it to a restrictive application of RD 16/2012, in the sense that for those centers with “one hundred beds or more in assisted care” there would only be two options for the pharmacy service, which would be to register the center as a hospital pharmaceutical depot and hire a hospital specialist pharmacist or to reach an agreement with the Health Department, with the public reference hospital becoming the drug depot.
In view of this, in order to study and discuss the issue, Adefarma Work organized a round table so that, freely and independently, groups of leading nursing homes and two commonly involved patients’ associations could express their opinions and concerns about the social and healthcare model and about what model we want to have. Exclusion would affect the daily life of patients and the activities of the centers, regardless of the number of beds, as has been repeatedly stated by the associations concerned (patients and centers):
- It is justified on the basis of misunderstood objectives, economic and public management.
- By forcing to have a pharmacist with a hospital specialty, it complicates the management of human resources in an already saturated system, experimenting and putting at risk a system that until now has been giving impeccable results.
- Not only is the capacity of the community pharmacist undervalued, but also the legitimate right of choice in centers (public and private management) and of users is undermined.
- Inequities between different Autonomous Communities and bed criteria would be incurred; despite the fact that they are all subject to the same Spanish Constitution (article 43) and the mixed public-private system would be bypassed.
- The right to free choice of service by each citizen is violated and the system is homogenized and institutionalized on a massive scale. Citizens are not hospitalized or hospitalized in social-health centers, it is their home, even if they are assisted, and they have the right to choose the pharmacy that provides them with the service.
- If a hospital is imposed, a new level of care is created, medication reconciliation is complicated and, for example, if the resident changes residence or goes on vacation alone or with his guardians, he is forced to go through a transition period and there is no guarantee that his medication will be available at his point of destination.
- The guarantee of continuous supply is jeopardized, reducing the diversification of supply. It would be broken unnecessarily, since the current system enjoys very high levels of quality and satisfaction and has never failed (never; neither in COVID, nor Filomena…).
The representatives of the Onacare L’Onada center explained that the centers have a whole arsenal of specific and individualized services, providing unique and specialized care, which is growing year after year, so it is not possible to apply regulatory interpretations that prevent these services from being developed efficiently, as this would make them unfeasible. They are services and ways of understanding the reality of patients from an updated, active, self-responsible lifestyle that makes guaranteeing and increasing the quality of life of its residents a priority. It is a matter of banishing the inertia of institutionalization, so that they do not abandon their environment, their home, and if they must, because they so wish, go to live in a center, they should not be homogenized.
Dr. José Luis Baquero began by recalling that in Spain 60% of people over 65 years of age suffer from at least one chronic disease, which means that most elderly people are patients, with osteoarticular pathology being one of the most prevalent. He approached the problem of aging from different aspects, such as the adaptation of the environment and the proposal of certification OAFI Space based on safety, comfort and quality of life parameters.
n any case, going into the central issue of the discussion, we cannot allow the citizens’ ability to choose to be bypassed, since they should not be treated as sick, regardless of whether the center has more or fewer beds, in one or another autonomous community, whether or not they are in assisted care, privately or publicly managed, etc. The idea is that these citizens, who have changed their place of residence, should have the same opportunities of choice as the rest of the citizens who are in their own homes, in order to guarantee the monitoring of adherence to treatment, traceability and accountability, and to avoid shortages, among many other aspects.
For his part, Rubén Martín, was very resolute; we only want freedom. He gave a series of criteria to make it clear that this is an interpretation that “I am sure that the Management Directorate will reach a consensus. That is our perception. He gave several pieces of information, such as the wording of Article 42, which is the one to which the Coordination Directorate alluded:
Article 42. Residential social services centers.
- Residential social services centers with one hundred beds or more in assisted care are obliged to establish their own hospital pharmacy service, authorized by the Regional Ministry of Health.
- However, those centers that establish agreements or arrangements with the Regional Ministry responsible for pharmaceutical services may have a drug deposit [without adding more, neither in a restrictive sense, nor in an extended sense].
- That is to say, it does not establish the impossibility of continuing to provide the service, it is necessary to establish how, but a priori “the regulations” do not oblige anything.
Regarding RD 16/2012, which was another argument:
- It is the RD of the co-payment, which is being repealed and applied in each Autonomous Community as deemed necessary.
- It is the RD of the copayment also hospital is not applied in any Autonomous Community.
- It is completely obsolete. It is from a time when the concept of “socio-health care” was not defined. Neither care center, nor assisted.
It is not indicated, therefore, that it should always be agreed in the sense of having to exclude the freedom of choice of each citizen, or in whom they delegate, in the sense of excluding any option.
It became clear in response to questions from those present and, therefore, affected, that there is no plan, since the answer to “what about emergencies, if hospital staff stop working at 3.30 p.m.? “Why change a system that works for another that we do not know if it will work?”, “Who is in charge of acute treatment?”, “What happens if the resident changes residence or Autonomous Community?”, “Should he/she request leave from the residence to reconcile medication if he/she leaves the residence and goes to live in the home of his/her relatives, for example on vacation?”, “Why create another level of care?”. The answer was always “because the regulations require it” or “we are going to see, we want to consult you”. We can only ask: What would have happened if this proposed system, once it has been made clear that it does not impose any regulations, had been implemented in the COVID with saturated hospitals? Moreover, who or what would have attended the residences at the time of flu saturation last fall?
He concluded with a series of reflections:
- What does this mean for users? Unnecessary risk of loss of quality and choice.
- What does this mean for the centers? Increased human resource costs, loss of quality and choice.
- What does it mean for pharmacies?
- In most cases it is the best way for professional development, since attending a nursing home, given the indirect costs involved, means a drop in the margin.
- Economic: by not being able to dedicate any of them now, neither in the present nor in the future, the goodwill is depreciated.
- Unjustified discrediting of the figure of the community pharmacist.
- What does this mean for the administration? Higher costs and risk of management collapse.
- What do we propose? That freedom of choice be respected, that citizens choose, as they have done up to now, and that we be allowed to compete.
Finally, remember that if you have osteopenia, osteoporosis or osteoarthritis or any other joint condition, or know someone who does, we encourage you to become a member of OAFI through our website. In addition to receiving free didactic and informative material, you will benefit from many other activities and you will be able to attend the Solidarity Clinic of Dr. Vergés and our nutritionist.
or by calling: (+34) 931 594 015.
We remain at your disposal!
Categories :