- Foundation
- Actions
- Osteoarthritis
- Actuality
- OAFI Radio/TV
- Get Involved
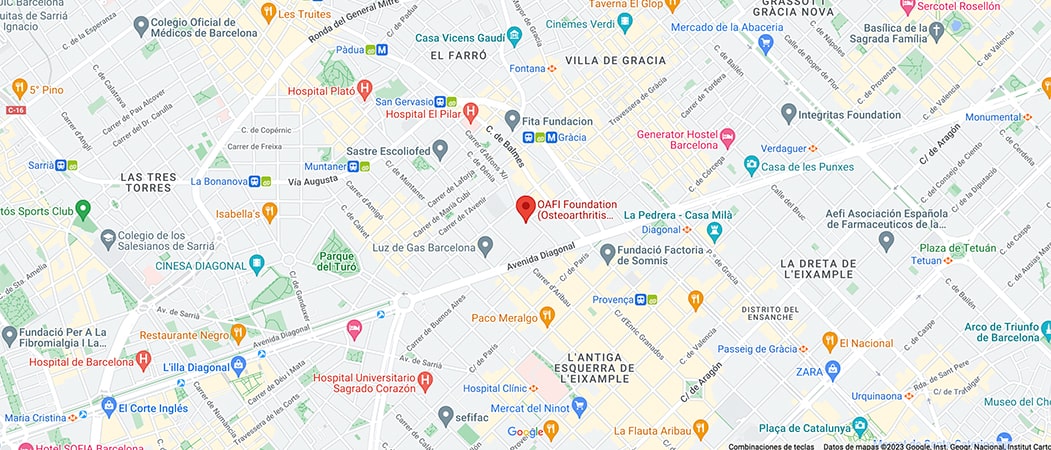
- Contact
-
-
-
OAFI
Osteoarthritis International FoundationC/ Tuset, 19 · 3º 2ª
08006 Barcelona
(+34) 931 594 015
info@oafifoundation.comSchedule:
Monday-Thursday 9AM-6PM
Friday 8AM-3PM
-
-
-

-

-

12 proposals to reduce the impact of obesity

- In Spain, more than 60% of the Spanish population has obesity or is at risk of suffering from it.
- It is the ninth country in Europe with one of the highest prevalences of excess weight.
- Only 69% of patients with obesity receive a diagnosis of obesity.
- Find out now the 12 proposals presented yesterday in Congress
With the aim of developing strategies to reduce the impact of obesity in our country, the report ‘Health and social situation of people with obesity in Spain’, drawn up by the Alliance for Obesity, made up of thirteen patient organizations and scientific societies, was presented at the Congress of Deputies. In the format of two round table discussions, the first with healthcare professionals and the second with parliamentary spokespersons from the Health Commission of the different majority groups, the organizations signing the document have called for the need to recognize obesity as a chronic and multifactorial disease in Spain, which, in the words of Victoria Buiza, spokesperson for the Alianza por la Obesidad and president of the association, “would be the first step towards the recognition of obesity as a chronic disease in Spain”. AB Híspalis Nacional, “not only would it improve prevention and care, but it would also boost research and investment in public health policies to address this growing problem”. In this way, he assures, “people with obesity will be able to form part of the Law of Guarantees and we will begin to be patients recognized by the Spanish healthcare system”.
This study aims to identify the barriers that hinder the management of the disease. Dr. Irene Bretón, a member of the Spanish Society of Endocrinology and Nutrition (SEEN), has warned that obesity is clearly underdiagnosed and that there is inadequate coordination in care between different healthcare professionals and clinical settings. “In general there is a lack of individualization and personalization of care to the patient’s needs, including emotional ones, and little information and training on this disease and its consequences.”
Thus, the main conclusion drawn from the report is that the lack of recognition of obesity as a disease inevitably leads to under-diagnosis. Despite scientific evidence supporting that obesity is a chronic disease, people with obesity tend to underestimate their actual weight status, resulting in significant delay in seeking medical care. The diagnostic process also presents challenges; according to the results obtained in the present study, only 69% of patients with obesity receive a diagnosis of obesity.
Obesity care and management
The study shows that one third of patients with obesity have not received specific care; only 67% of patients with obesity receive some type of health care for it, being attended on average by 2 or 3 specialists. Professionals from specialties such as endocrinology, primary care and nutrition are the most frequently involved, while equally relevant disciplines such as psychology or internal medicine tend to play a secondary role in care for them, leaving critical patient needs unmetii. These deficiencies in coordination and continuity of care and the absence of a comprehensive multidisciplinary approach compromise the quality of health care. Specialized psychological care and behavioral therapy are an example. These disciplines are highlighted as an essential component in the approach to obesity, yet 71% of the study participants have not had access to this type of treatment, despite the fact that 56% of them consider that it would have been beneficial and only 29% have had access to specialized psychological care.
Stigma, the other great pending challenge to alleviate obesity
Stigmatization in the healthcare and social settings is another challenge that negatively affects the quality of healthcare and the well-being of patients, including the work, educational, family and social settings in general. This prejudice arises from the widespread perception that obesity is the result of a lack of willpower and bad habits.iii, as well as negative stereotypes related to obesity.ivv. In this sense, Dr. Alberto Lecube, member of the Spanish Society for the Study of Obesity (SEEDO), explained that obesity is neither a vice nor a moral disease. “A person does not choose to be obese, but rather the disease chooses him or her”, which is why he believes that “we cannot continue to accept that obesity continues to be an open door to inequity and discrimination throughout the healthcare process”. This expert has assured that, in addition to changing lifestyle, which is essential, it is necessary to evaluate all the tools that medicine offers to deal with it and to attend to the individual needs of each individual. Dr. Lecube emphasizes that the strategies should not be mutually exclusive: “we can have patients with obesity in whom we combine different interventions depending on the moment and state of health. Incorporating bariatric surgery in the prioritization lists of healthcare systems, expanding its offer and guaranteeing adequate follow-up after surgery is a priority in the fight against obesity”.
12 proposals to reduce the impact of obesity in Spain
In the face of the solid evidence supporting the high prevalence of obesity, its worrying upward trend, its significant impact on both the healthcare system and the economy (obesity accounts for 9.7% of total healthcare expenditure and reduces labor productivity by the equivalent of 479,000 working days per year), its wide range of associated comorbidities and its negative impact on quality of life, obesity stands out as a pressing challenge in Spanish public health. 000 working days per year), its wide range of associated comorbidities and its negative impact on quality of life, obesity stands as a pressing challenge in Spanish public health for which this strategic alliance proposes 12 proposals that focus on more effective care and the promotion of a comprehensive approach to the disease to mitigate the impact on the health and well-being of those affected:
- Promote the real recognition of obesity as a chronic disease.
- Develop awareness and sensitization campaigns on obesity.
- Develop health education and promotion programs in schools.
- To carry out training and awareness actions for health professionals.
- Implement early detection programs for overweight in a systematic way.
- Establish comprehensive diagnostic protocols.
- Establish personalized and comprehensive treatment and follow-up protocols.
- Establish specific multidisciplinary teams to address obesity.
- Incorporate bariatric surgery in the prioritization lists of the health systems, expand its offer and guarantee adequate follow-up after surgery.
- Establish communication and coordination protocols between the different health professionals.
- Expand access to specialized psychological care and behavioral therapy.
- Promote patient co-responsibility through health information and education.
Obesity in numbers
Obesity has increased almost threefold in prevalence since 1975, representing, without a doubt, a growing global health challenge. Currently, it is estimated that more than 988 million adults suffer from obesity.ix, and this figure is expected to double by 2030.x. In Spain, more than 60% of the Spanish population has obesity or is at risk of suffering from it.xixii. Thus, Spain is the ninth country in Europe with one of the highest prevalence of excess weight.xiii.
About the Alliance for Obesity
In view of the growing impact of obesity on public health and the population of Spain, a strategic alliance composed of thirteen patient organizations and scientific societies has been formed with the fundamental purpose of promoting the visibility and defending the rights of people facing obesity in Spain. This central objective seeks to establish obesity as a chronic disease that requires a comprehensive and multidisciplinary approach, as well as to improve the healthcare provided to those who suffer from it. To achieve this objective, three specific actions have been outlined:
- To generate evidence on the impact of obesity on people who suffer from it.
- To make available to public administrations proposals for improvement in the approach to obesity.
- To influence health authorities on the importance of obesity being recognized as a chronic disease.
*Asociación Bariátrica Híspalis Nacional, Asociación de Pacientes Bariátricos y Obesidad (AB Híspalis), Asociación Española de Cáncer de Tiroides (AECAT), Asociación española de Gastroenterología (AEG), Asociación de Enfermos de Esófago de Barret (ASENBAR), Cardioalianza, Federación Española de Diabetes (FEDE), Federación Nacional de Enfermos y Trasplantados Hepáticos (FNETH), Osteoarthritis Foundation International (OAFI), Sociedad Española de Cirugía de la Obesidad (SECO), Sociedad Española para el Estudio de la Obesidad (SEEDO), Sociedad Española de
Endocrinología y Nutrición (SEEN), Sociedad Española de Médicos Generales y de Familia (SEMG), Sociedad Española de Medicina Interna (SEMI), con la colaboración de Novo Nordisk.
References:
i Lecube, A., Sánchez, E., Monereo, S., Medina-Gómez, G., Bellido, D., García-Almeida, J.M., de Icaya, P.M., Malagón, M.M., Goday, A., and Tinahones, F.J. (2020). Factors Accounting for Obesity and Its Perception among the Adult Spanish Population: Data from 1000 Computer-Assisted Telephone Interviews. Obesity Facts, 13(4):322-332.
ii Baile, J.I., González-Calderón, M.J., Palomo, R., and Rabito-Alcón, M.F. (2020). Psychological Intervention of Obesity: Development and Perspectives. Revista de Diagnóstico Psicológico, Psicoterapia y Salud, 1(11):1-14.
iii Flint, S.W., Nobles, J., Gately, P., and Sahota, P. (2018). Weight Stigma and Discrimination: A Call to Media. The Lancet, 6(3):169-170.
iv Turner, M.M., Ford, L., Somerville, V., Javellana, D., Day, K.R., and Lapinski, M.K. (2020). The Use of Stigmatizing Messaging in Anti-Obesity Communications Campaigns: Quantification of Obesity Stigmatization. Communication Reports, 33(3):107-120.
v Bristow, C., Meurer, C., Simmonds, J., and Snell, T. (2020). Anti-Obesity Public Health Messages and Risk Factors for Disordered Eating: A Systematic Review. Health Promotion International, 35(6):1551-1569.
vi Organisation for Economic Cooperation and Development. (2019). The Heavy Burden of Obesity: The Economics of Prevention. Disponible en: https://www.oecdilibrary.org/sites/67450d67en/index.html?itemId=/content/publication/67450d67-en.
Consultado: 5 de octubre de 2023.
vii Hernáez, A., Zomeño, A.D., Dégano, I.R., Pérez-Fernández, S., Goday, A., Vila, J., Civeira, F., Moure, R., and Marrugat., J. (2019). Exceso de Peso en España: Situación Actual, Proyecciones para 2030 y Sobrecoste Directo Estimado para el Sistema Nacional de Salud. Revista Española de Cardiología, 72(11):916-924.
viii Okunogbe, A., Nugent, R., Spencer, G., Ralston, J., and Wilging, J. (2021). Economic Impacts of Overweight and Obesity: Current and Future Estimates for Eight Countries. BMJ Global Health, 6(10).
ix World Obesity Federation’s ‘Obesity Atlas 2023, March 2023. Consultar publicación en World_Obesity_Atlas_2023_Report.pdf. Última visualización 11.09.2023
x World Obesity Federation. (2022). World Obesity Atlas 2022. Disponible en: https://s3-eu- west1.amazonaws.com/wof-files/World_Obesity_Atlas_2022.pdf. Consultado: 5 de octubre de 2023.
xi Instituto Nacional de Estadística. (2017). Índice de Masa Corporal Población Infantil según Sexo y Comunidad Autónoma. Población de 2 a 17 años. Disponible en: https://www.ine.es/jaxi/Tabla.htm?path=/t15/p419/a2017/p06/&file=01011.px. Consultado: 5 de octubre de 2023. xii Instituto Nacional de Estadística. (2020). Índice de Masa Corporal por CCAA y Periodo. Población de 18 y más años. Disponible en: https://www.ine.es/jaxi/Tabla.htm?path=/t00/ICV/dim3/l0/&file=33101.px. Consultado: 5 de octubre de 2023.
xiii World Health Organizarion. (2022). WHO European Regional Obesity Report 2022. Disponible en: https://iris.who.int/bitstream/handle/10665/353747/9789289057738-eng.pdf. Consultado: 5 de octubre de 2023.
Article courtesy of Alianza Multidisciplinar por la Obesidad.
Remember that in OAFI we have a nutrition and dietetics service, and you can make an appointment only by calling (+34) 931 594 015.