- Foundation
- Actions
- Osteoarthritis
- Actuality
- OAFI Radio/TV
- Get Involved
- Contact
-
-
-
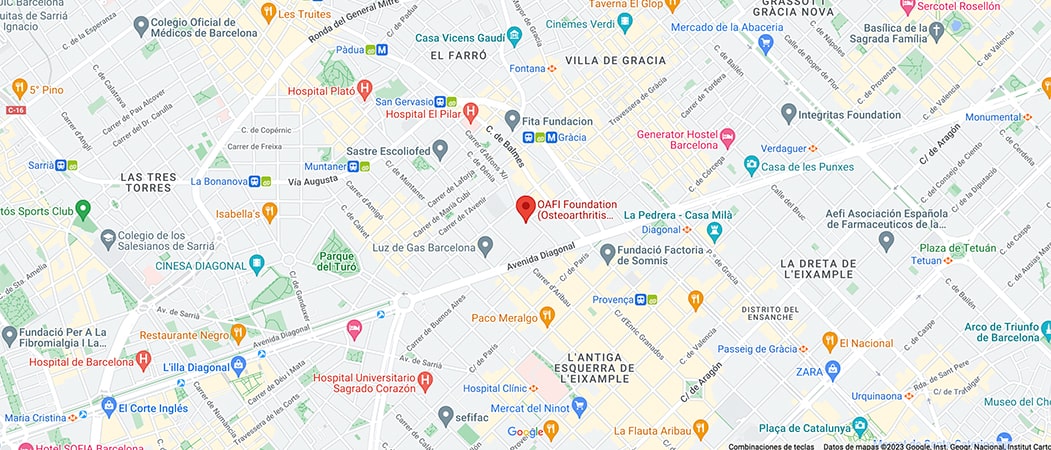
OAFI
Osteoarthritis International FoundationC/ Tuset, 19 · 3º 2ª
08006 Barcelona
(+34) 931 594 015
info@oafifoundation.comSchedule:
Monday-Thursday 9AM-6PM
Friday 8AM-3PM
-
-
-

-

-

CHAPTER 1: Bone Health and Vitamin D. What is it and why is it so important?

- The misnamed Vitamin D is actually a hormone essential for the proper functioning of multiple tissues and organs in the human body.
- Vitamin D (Vit D) is well known for its actions at the musculoskeletal level, but it also has multiple functions, called pleiotropic, in other organs and systems such as the immune system, the central nervous system or the endocrine system among others.
Role in the central nervous system:
The Vit D has neuroprotective and anti-inflammatory effects at the level of the brain being able to protect it against toxins, protecting the survival of neurons, involvement in the release of neurotransmitters such as dopamine, GABA, serotonin[i][ii]54 and helping to reduce inflammation of the nervous system thanks to its role in the release of substances called anti-inflammatory cytokines. There is already abundant evidence of the relevant role of Vit D in diseases such as multiple sclerosis, Alzheimer’s disease, Parkinson’s disease or epilepsy patients treated with antiepileptic drugs, among others. This indicates that the role of Vit D is much broader and more relevant than we might initially expect.
Role in the immune system:
The activity of Vit D at the level of the immune system has also been extensively studied. Vit D acts as an immunomodulator in such a way that it helps the innate immune system (that which presents the immediate response to infections) and at the same time participates in the regulation of the adaptive immune response (that which is associated with autoimmune diseases such as multiple sclerosis). Given the relevant role of Vit D on the immune system, a large number of clinical studies have been performed during the COVID-19 epidemic[i] showing that Vit D could improve the immune response to infections, reduce recovery time, reduce hospitalization rate, reduce ICU admission rate and even mortality. The role of Vit D in other types of infections such as acute respiratory infections typical of winter (colds, flus…) has also been demonstrated in other clinical studies.
In the case of COVID-19, multiple studies have been performed in recent years. These studies have suggested that low levels of Vit D (<20 ng/ml) significantly increase the risk of COVID-19 infection in adults[ii] [iii] [iv]. In fact it was shown in 2021 in a study of 1 million adults, that Vit D deficiency was associated with increased severity of COVID and 3-fold increased likelihood of death[v].
Another more recent study showed an 80% increased risk of infection in people with low levels of Vit D[vi]. Other observational studies further suggest that Vit D deficiency is associated with a doubling of the hospitalization rate and a tripling of the ICU admission rate and mortality rate[vii] [viii] [ix].
Role of the Vit D in the musculoskeletal system:
The importance of internal Vit D synthesis is such that it has led to evolutionary pressure on man to reduce skin pigmentation as humans migrated from Africa to Europe and northern countries[i] and is considered an important evolutionary factor of the species such that Vit D deficiency occurring in northern latitudes resulted in a loss of bone strength and a poorer immune system.
The skeleton is a dynamic, metabolically active and functionally diverse organ that is continuously remodeling through 2 coordinated processes: bone resorption (bone destruction) and bone formation[ii] [iii]. Imbalance of these processes can cause diseases such as rickets, osteomalacia, osteoclerosis and osteoporosis[iv] [v].
Throughout life, the bone skeleton is subjected to a continuous and dynamic process of construction-deconstruction (in what is called bone modeling and remodeling) that aims to repair bone damage, prevent accumulation of hyper-mineralization, and maintain balance in calcium and phosphate deposits. These processes are so dynamic that it is estimated that up to 10% of the bone skeleton is renewed each year[vi].
Both adequate muscle strength and mass and proper bone formation are essential to avoid the dreaded falls and fractures, so maintaining proper osteo-muscular health is important, especially for people with osteoporosis or in the elderly.
Maintaining optimal Vit D levels is important as Vit D is known to play an important role in all these bone remodeling processes as it is involved in:
- The processes of new bone formation.
- In the bone remodeling cycle as it ensures the availability of calcium[vii] and phosphate[viii] to mineralize new bone.
- It helps to ensure that there are sufficient bone-forming cells (called osteoblasts) [ix] [x].
- Reduction of bone fractures.
- Improving bone density to prevent or reduce osteoporosis.
- Aids bone repair after fracture[xi].
It has also been shown that Vit D is essential for muscle function as it promotes[xii] [xiii] [xiii]:
- Musculoskeletal cell proliferation and differentiation.
- Musculoskeletal cell metabolism.
- Muscle function, mass and strength.
- Muscle development and repair.
- It also plays a role in the inflammatory response of muscle.
Article courtesy of Dr. Esperanza Regueras. Pharmacist and Doctor of Pharmacy. CEO and scientific director of Advantal Pharma.
Bibliography
[1] Seyedi M, Gholami F, Samadi M, Djalali M, Effatpanah M, Yekaninejad MS, Hashemi R, Abdolahi M, Chamari M, Honarvar NM. The Effect of Vitamin D3 Supplementation on Serum BDNF, Dopamine, and Serotonin in Children with Attention-Deficit/Hyperactivity Disorder. CNS Neurol Disord Drug Targets. 2019;18(6):496-501. doi: 10.2174/1871527318666190703103709. PMID: 31269890.
[2] Murthi P, Davies-Tuck M, Lappas M, Singh H, Mockler J, Rahman R, Lim R, Leaw B, Doery J, Wallace EM, Ebeling PR. Maternal 25-hydroxyvitamin D is inversely correlated with foetal serotonin. Clin Endocrinol (Oxf). 2017 Mar;86(3):401-409. doi: 10.1111/cen.13281. Epub 2016 Dec 19. PMID: 27862146.
[3] Entrenas Castillo M, Entrenas Costa LM, Vaquero Barrios JM, et al. Effect of calcifediol treatment and best available therapy versus best available therapy on intensive care unit admission and mortal- ity among patients hospitalized for COVID-19: a pilot randomized clinical study. J Steroid Biochem Mol Biol. 2020;203:105751.
[4] KaufmanHW,NilesJK,KrollMH,BiC,HolickMF.SARS-CoV-2positiv- ity rates associated with circulating 25-hydroxyvitamin D levels. PLoS One. 2020;15(9):e0239252.
[5] Merzon E, Tworowski D, Gorohovski A, et al. Low plasma 25(OH) vitamin D level is associated with increased risk of COVID- 19 infection: an Israeli population-based study. FEBS J. 2020; 287(17):3693-3702.
[6] Brenner H. Vitamin D supplementation to prevent COVID-19 infec- tions and deaths—accumulating evidence from epidemiological and intervention studies calls for immediate action. Nutrients. 2021;13(2):411.
[7] Akbar MR, Wibowo A, Pranata R, Setiabudiawan B. Low serum 25- hydroxyvitamin D (Vitamin D) Level is associated with susceptibility to COVID-19, severity, and mortality: a systematic review and meta- analysis. Front Nutr. 2021;8:660420.
[8] TeshomeA,AdaneA,GirmaB,MekonnenZA.Theimpactofvitamin D level on COVID-19 infection: systematic review and meta-analysis. Front Public Health. 2021;9:624559.
[9] Charoenngam N, Ponvilawan B, Rujirachun P, Wattanachayakul P. Association of vitamin D Status with hospital morbidity and mortal- ity in adult hospitalized patients with COVID-19. Endocr Pract. 2021; 27(4):271-278.
[10] Angelidi AM, Belanger MJ, Lorinsky MK, et al. Vitamin D status is associated with in-hospital mortality and mechanical ventilation: a cohort of COVID-19 hospitalized patients. Mayo Clin Proc. 2021; 96(4):875-886.
[11] PetrelliF,LucianiA,PeregoG,etal.Therapeuticandprognosticrole of vitamin D for COVID-19 infection: a systematic review and meta- analysis of 43 observational studies. J Steroid Biochem Mol Biol. 2021; 211:105883.
[12] Carlberg C. Nutrigenomics of Vitamin D. Nutrients. 2019 Mar 21;11(3):676. doi: 10.3390/nu11030676. PMID: 30901909; PMCID: PMC6470874
[13] N.A. Sims, T.J. Martin, Coupling the activities of bone formation and resorption: a multitude of signals within the basic multicellular unit, Bonekey. Rep. 3 (2014) 481.
From OAFI we recommend following the advice, always under the supervision of your trusted physician.
*Image illustrating the article by Michele Blackwell