- Foundation
- Actions
- Osteoarthritis
- Actuality
- OAFI Radio/TV
- Get Involved
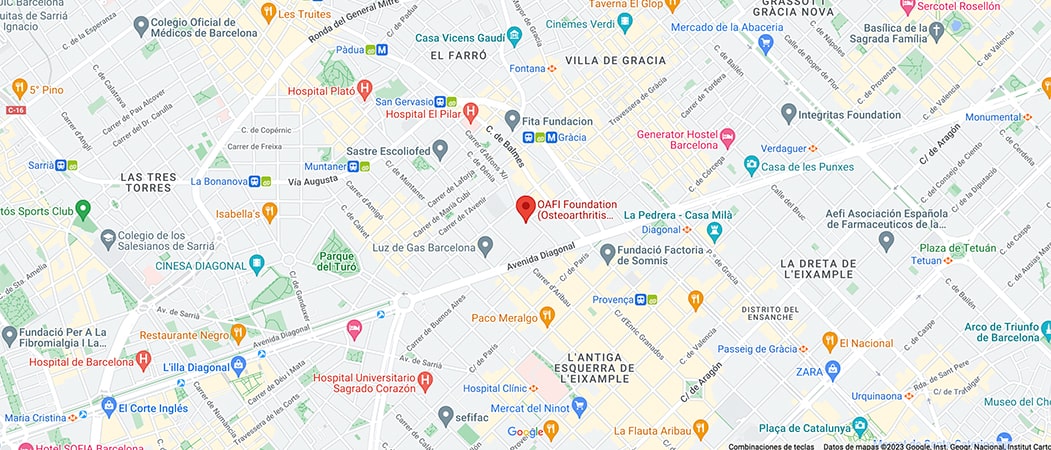
- Contact
-
-
-
OAFI
Osteoarthritis International FoundationC/ Tuset, 19 · 3º 2ª
08006 Barcelona
(+34) 931 594 015
info@oafifoundation.comSchedule:
Monday-Thursday 9AM-6PM
Friday 8AM-3PM
-
-
-

-

-

CHAPTER 2. Bone Health and Vitamin D: Vitamin D in Osteoporosis

- Osteoporosis is a metabolic disease that weakens bone architecture and reduces bone density and strength resulting in an increased risk of fractures[i].
Figure 1: Comparison of internal structure in healthy bone and osteoporosis
Healthy bone has a more compact structure whereas in osteoporosis there is less bone density.
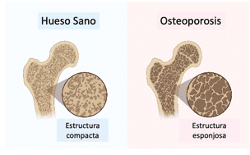
Figure 2: Common symptoms of osteoporosis
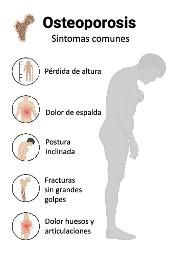
Osteoporosis is a very common disease and it is estimated that 27.6 million people in Europe suffer from it. One of the main consequences of osteoporosis are the so-called osteoporotic fractures, which occur in these patients even with small blows or falls. These fractures are very frequent and can affect up to 1/3 of women and 1/5 of men over 50 years of age[i].
Worldwide, osteoporosis affects some 200 million people and is associated with 9 million fractures per year[i] and it is estimated that by the year 2050, 21 million hip fractures may occur annually due to this cause.[ii].
Vit D deficiency is one of the factors contributing to the development of osteoporosis. When the concentration of Vit D is less than 20 ng/ml, there is an increased risk of femoral fractures and non-vertebral fractures in older patients and postmenopausal women.[i][ii].
The elderly are highly vulnerable to osteoporotic and fragility fractures, which pose a high health and economic burden. The impact of these fractures, especially hip fractures, is enormous.[i] [ii] [iii] [iv] [v].:
- 30% of patients become permanently disabled,
- 40% lose the ability to walk independently.
- 80% become dependent for daily activities after fracture.
- And produce a 20% excess mortality at 1 year.
As we have seen, Vit D deficiency is associated with worse muscle function, lower bone density and, therefore, increased risk of falls. In fact, studies have shown that, in patients with osteoporosis and fragility fracture, including hip fracture, there is a high prevalence of Vit D deficiency.[i] [ii].
Vit D not only reduces the risk of falls, but also improves fracture healing by facilitating bone regeneration processes, as seen in several studies.[iii].
Supplementation with Vit D, therefore, forms part of the basic treatment of osteoporosis and is recognized as such in the guidelines of several scientific societies. For example, the SIMMONS[1] recommended in 2022[i] achieve optimal Vit D blood levels between 20-50 ng/ml and supplement, when necessary, with cholecalciferol between 800 and 2,000 IU per day. In other hand, the ESCEO[2], also in 2022[ii] recommends supplementing with Vit D between 200 and 2,000 IU per day to achieve at least 20 ng/ml.
[1] (Society for osteoporosis, mineral metabolism and bone diseases.)
[2] (European Society for Clinical and Economic Aspects of Osteoporosis, Osteoarthritis and Musculoskeletal Diseases.)
[1] (European Food Safety Authority)
EFSA recommendations[1] indicate that in adults the recommended dose of Vit D supplementation is between 600 and a maximum of 4,000 IU per day.
Conclusions:
- Vitamin D is a hormone necessary for the proper functioning of various systems (nervous system, immune system) as well as for bone turnover-mineralization and proper bone density.
- Vitamin D also supports muscle function, mass and strength.
- Osteoporosis is a common disease that increases the risk of falls and fractures.
- Vitamin D supplementation can help people with osteoporosis by its benefits on bone and muscles, reducing the risk of falls and fractures.
- Scientific societies recommend Vitamin D supplementation for osteoporosis patients to achieve optimal levels.
A dose of 600 to 800 IU per day of Vit D is adequate for most patients to maintain optimal Vit D levels. This dose should be increased if necessary to achieve optimal Vit D blood levels (between 30-50 ng/ml).
Article courtesy of Dr. Esperanza Regueras. Pharmacist and Doctor of Pharmacy. CEO and scientific director in Advantal Pharma.
Bibliography
[1] (Agencia Europea de Seguridad Alimentaria)
[1] (Sociedad de osteoporosis, metabolismo mineral y enfermedades óseas)
[2] (Sociedad Europea para aspectos clínicos y económicos de la osteoporosis, osteoartritis y enfermedades musculo-esqueléticas)
[i] Bertoldo F, Cianferotti L, Di Monaco M, Falchetti A, Fassio A, Gatti D, Gennari L, Giannini S, Girasole G, Gonnelli S, Malavolta N, Minisola S, Pedrazzoni M, Rendina D, Rossini M, Chiodini I. Definition, Assessment, and Management of Vitamin D Inadequacy: Suggestions, Recommendations, and Warnings from the Italian Society for Osteoporosis, Mineral Metabolism and Bone Diseases (SIOMMMS). Nutrients. 2022 Oct 6;14(19):4148. doi: 10.3390/nu14194148. PMID: 36235800; PMCID: PMC9573415.
[ii] Chevalley T, Brandi ML, Cashman KD, Cavalier E, Harvey NC, Maggi S, Cooper C, Al-Daghri N, Bock O, Bruyère O, Rosa MM, Cortet B, Cruz-Jentoft AJ, Cherubini A, Dawson-Hughes B, Fielding R, Fuggle N, Halbout P, Kanis JA, Kaufman JM, Lamy O, Laslop A, Yerro MCP, Radermecker R, Thiyagarajan JA, Thomas T, Veronese N, de Wit M, Reginster JY, Rizzoli R. Role of vitamin D supplementation in the management of musculoskeletal diseases: update from an European Society of Clinical and Economical Aspects of Osteoporosis, Osteoarthritis and Musculoskeletal Diseases (ESCEO) working group. Aging Clin Exp Res. 2022 Nov;34(11):2603-2623. doi: 10.1007/s40520-022-02279-6. Epub 2022 Oct 26. PMID: 36287325; PMCID: PMC9607746.
[i] Bouillon R, Marcocci C, Carmeliet G, Bikle D, White JH, Dawson-Hughes B, Lips P, Munns CF, Lazaretti-Castro M, Giustina A, Bilezikian J (2019) Skeletal and extraskeletal actions of vitamin D: current evidence and outstanding questions. Endocr Rev 40:1109–1151
[ii] Bischoff-Ferrari HA, Can U, Staehelin HB, Platz A, Henschkowski J, Michel BA, Dawson-Hughes B, Theiler R (2008) Severe vitamin D deficiency in Swiss hip fracture patients. Bone 42:597–602
[iii] Chevalley T, Brandi ML, Cavalier E, Harvey NC, Iolascon G, Cooper C, Hannouche D, Kaux JF, Kurth A, Maggi S, Maier G, Papavasiliou K, Al-Daghri N, Sosa-Henríquez M, Suhm N, Tarantino U, Reginster JY, Rizzoli R. How can the orthopedic surgeon ensure optimal vitamin D status in patients operated for an osteoporotic fracture? Osteoporos Int. 2021 Oct;32(10):1921-1935. doi: 10.1007/s00198-021-05957-9. Epub 2021 May 20. PMID: 34013461; PMCID: PMC8134831.
[i] Schurch MA, Rizzoli R, Mermillod B, Vasey H, Michel JP, Bonjour JP (1996) A prospective study on socioeconomic aspects of fracture of the proximal femur. J Bone Miner Res 11:1935– 1942
[ii] Johnell O, Kanis JA (2004) An estimate of the worldwide preva- lence, mortality and disability associated with hip fracture. Osteoporos Int 15:897–902
[iii] Piscitelli P, Neglia C, Feola M, Rizzo E, Argentiero A, Ascolese M, Rivezzi M, Rao C, Miani A, Distante A, Esposito S, Iolascon G, Tarantino U (2020) Updated incidence and costs of hip frac- tures in elderly Italian population. Aging Clin Exp Res 32:2587– 2593
[iv] Pedersen AB, Ehrenstein V, Szepligeti SK, Lunde A, Lagerros YT, Westerlund A, Tell GS, Sorensen HT (2017) Thirty-five- year trends in first-time hospitalization for hip fracture, 1-year mortality, and the prognostic impact of comorbidity: a Danish nationwide cohort study, 1980-2014. Epidemiology 28:898–905
[v] Borgstrom F, Karlsson L, Ortsater G et al (2020) Fragility frac- tures in Europe: burden, management and opportunities. Arch Osteoporos 15:59
[i] Aspenberg P, Johansson T. Teriparatide improves early callus formation in distal radial fractures. Acta Orthop. 2010;81(2):234–6. doi: 10.3109/17453671003761946.
[ii] Garnero P, Munoz F, Sornay-Rendu E, Delmas PD. Associations of vitamin D status with bone mineral density, bone turnover, bone loss and fracture risk in healthy postmenopausal women. The OFELY study. Bone. 2007;40(3):716–22. doi: 10.1016/j.bone.2006.09.026
[i] Johnell O., Kanis J.A. An Estimate of the Worldwide Prevalence and Disability Associated with Osteoporotic Fractures. Osteoporos. Int. 2006;17:1726–1733. doi: 10.1007/s00198-006-0172-4.
[ii] Pisani P., Renna M.D., Conversano F., Casciaro E., Di Paola M., Quarta E., Muratore M., Casciaro S. Major Osteoporotic Fragility Fractures: Risk Factor Updates and Societal Impact. World J. Orthop. 2016;7:171–181. doi: 10.5312/wjo.v7.i3.171.
[i] Kenkre JS, Bassett J. The bone remodelling cycle. Ann Clin Biochem. 2018 May;55(3):308-327. doi: 10.1177/0004563218759371. Epub 2018 Mar 4. PMID: 29368538.
[i] Ryan JW, Anderson PH, Turner AG, Morris HA. Vitamin D activities and metabolic bone disease. Clin Chim Acta. 2013 Oct 21;425:148-52. doi: 10.1016/j.cca.2013.07.024. Epub 2013 Jul 30. PMID: 23911750.
*From OAFI we recommend following the advice, always under the supervision of your trusted physician.
*Illustrative image of the article by Towfiqu Barbhuyda
Categories :