- Foundation
- Actions
- Osteoarthritis
- Actuality
- OAFI Radio/TV
- Get Involved
- Contact
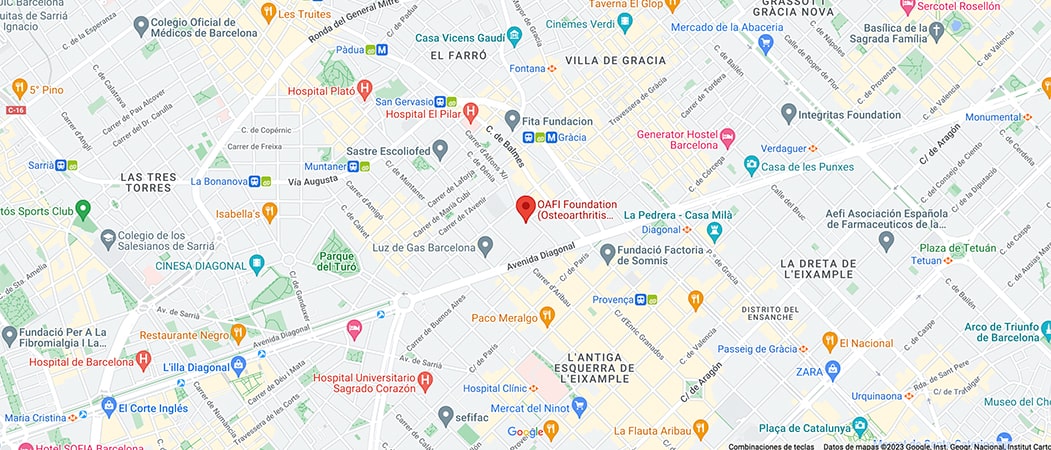
OAFI
Osteoarthritis International FoundationC/ Tuset, 19 · 3º 2ª
08006 Barcelona
(+34) 931 594 015
info@oafifoundation.comSchedule:
Monday-Thursday 9AM-6PM
Friday 8AM-3PM
-

-

OAFI Release About Coronavirus/Covid-19

The U.S .Centers for Disease Control and Prevention (CDC) have updated their recommendations for people who are at increased risk for complications from COVID-19, including people over the age of 60 and people with serious chronic medical conditions. “Stay home as much as possible” and “avoid the crowds”.
According to the website from the CDC, “Older Adults and People Who Have Medical Chronic Conditions, such as heart, lung, or kidney disease, could have an increased risk of contracting COVID-19 disease severely. The preliminary data suggests that older people are twice as likely to develop the most severe form of the disease caused by the COVID-19 virus.”
The CDC website says, “If you are at increased risk for complications from COVID-19 because of age or because you have a serious underlying medical condition, it is especially important that you take steps to reduce the risk of infection.” In addition, it recommends taking additional protection measures if COVID-19 is spreading in your community such as maintaining an adequate distance between you and other people, staying home as much as possible and avoiding crowds, especially in poorly ventilated spaces.
We ask Dr. Michael George, a rheumatologist and epidemiologist who studies infections in patients with autoimmune disease, who should follow these recommendations. His answer: “The more at risk you are, the more you should consider these recommendations”.
According to the expert, these new measures apply particularly to those with more illnesses, severe or have been hospitalized in the past with a respiratory infection or have interstitial lung disease, COPD, or asthma, for example. (See below for more details on risk factors.)
People with osteoarthritis, or non-autoimmune types of arthritis, which have risk factors, such as age (over 60 years) or a serious underlying medical condition must also follow CDC guidelines on how to avoid crowds.
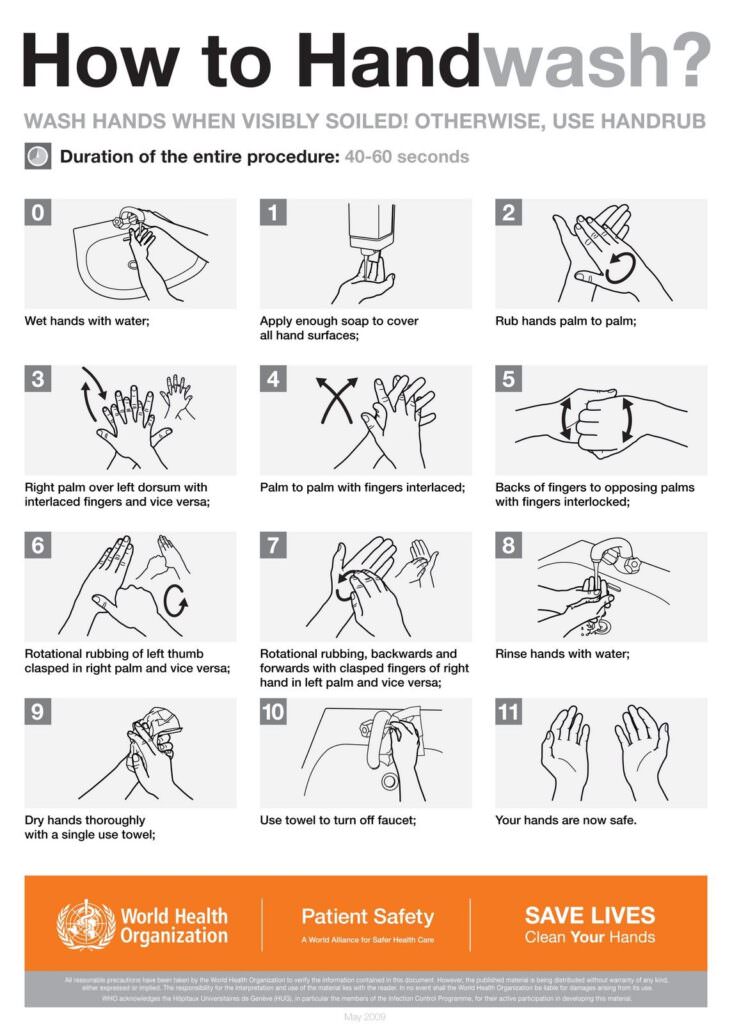
And, adds Dr. George, “Everyone should follow general precautions,” such as washing hands, not touching their faces, eyes, nose or mouth.
P: What is a Coronavirus?
A: Coronaviruses are a large family of viruses that can cause everything from colds to severe pneumonia. Some point to your nose, so you get a cold and a sore throat. Others, such as the new coronavirus that causes COVID-19, adhere to cells in the lungs.
Q: What are the COVID-19 symptoms?
A: Most of the people, about 80% or more, have mild symptoms similar to a seasonal cold or flu. Fever, cough, and shortness of breath may appear two to 14 days after infection. (An unpublished study suggests that the incubation period may last an additional week). A small number of people develop severe pneumonia, and some become seriously ill. Some people who test positive for COVID-19 never get sick, but they can transmit the virus.
Q: How does the virus spread?
A: Like seasonal colds and flu, the new coronavirus spreads through the droplets thrown out when a person coughs or sneezes. People can also contract the virus when they touch a contaminated surface such as a counter, handrails or doorknob and then touch their eyes, nose or mouth. The virus is unlikely to survive on hard surfaces for a long time, although it is not clear how long, says Dr. Timothy Brewer, professor of epidemiology at the University of California, Los Angeles. Isopropyl alcohol, hydrogen peroxide, and bleach can effectively kill surface viruses in about one minute. Soap and water, as well as disinfectants like Sanytol, also work, although not as well.
Q: Am I more likely to get COVID-19 if I have autoimmune or inflammatory arthritis?
A: We still do not have all the information about this virus, says Dr. Kevin Winthrop, an infectious disease epidemiologist at the at the University of Science and Medicine School in Portland, Oregon. However, in general, people with autoimmune or inflammatory arthritis who have high disease activity appear to be at increased risk of infection due to increased immune dysregulation.
For COVID-19 and seasonal flu, we know that older adults and those with pre-existing health problems, especially cardiovascular disease, diabetes and high blood pressure, and those who have been previously hospitalized with infections, are at increased risk.
Experts emphasize that one of the main concerns for people with autoimmune disease who contract seasonal flu or COVID-19 is secondary bacterial infection, or complications, that may follow the original viral infection.
For these reasons, it is important that you immediately call your doctor or the toll-free numbers enabled for this purpose by the different Autonomous Communities if you think that you have been exposed or have flu-like symptoms. Be sure to indicate that you are taking immunosuppressive medications. (Read below about immunosuppressive medications and risk).
Q: Am I more at higher risk of infection when taking immunosuppressive drugs?
A: We do not know whether taking immunosuppressive medications further increases the risk of contracting COVID-19. But Dr. Michael George, a rheumatologist and an assistant professor of medicine and epidemiology at the University of Pennsylvania in Philadelphia says that, regarding viruses in general, some data suggests that certain drugs used to treat autoimmune or inflammatory arthritis, such as organic products (eg Remicade, Enbrel and Cimzia), JAK inhibitors (Xeljanz, Olumiant and Rinvoq) and corticosteroids (prednisone), may contribute to an increased risk or severity of infection viral. A recent study in people with cardiovascular disease found that hydroxychloroquine (Plaquenil) does not increase the risk of infection and methotrexate increases the risk of infection only slightly.
The concern with immune suppression is that the virus could replicate more freely and cause more severe or extensive disease, says Dr. Winthrop. For this reason, it is important, if you are taking these medications,to contact your doctor immediately if you think you have been exposed or have flu-like symptoms. (See question on symptoms). Be sure to indicate that you are taking immunosuppressive medications.
Experts warn patients not to stop or change the dose of the drug without calling your doctors.
Q: Can my pet infect me with the COVID-19?
A: The World Health Organization (WHO) says there is no evidence that cats and dogs can contract or transmit the coronavirus to people. There is a lot of misinformation about how the virus started, and some people suggest it was made in a laboratory. That is not true. Based on previous coronavirus outbreakes and the virus genome, experts say it appears to have started in a wild animal, probably a bat or pangolin.
Q: How deadly is the virus?
A: It is difficult to say. Estimates are likely to change as milder cases are detected or reported. When people with mild illness are not counted, the virus can seem more deadly than it is. As of March 1, 2020, there were 87,508 confirmed cases worldwide and 2,990 deaths, according to the Johns Hopkins University Science and Systems Engineering Center in Baltimore, which is closely following the spread of the virus in the world. In comparison, CDC data estimates that in the U.S. alone, 18,000 to 46,000 people have died of seasonal flu since October 2019.
Q: What should I do if I think I have this virus?
A: Immediately call your doctor or the toll-free numbers authorized for this purpose by the different Autonomous Communitie, and be sure to tell them what type of medications you are taking. Your doctor will probably tell you to treat mild symptoms the same way you would with a cold or flu: rest, drink fluids, and stay isolated from others. If your symptoms are moderate or severe, they will probably send you to the hospital, where they will monitor you for complications, such as pneumonia.
Q: If I am infected, is my family at risk?
If you are infected, you should isolateyourself at your home for at least 14 days. If possible, have others use a separate toilet and do not handle or touch objects that you have touched without gloves. Cough and sneeze into the crook of your elbow, not your hands. Everyone should wash their hands thoroughly and frequently (if possible, use separate sinks).
Don’t worry or panic, but take steps to protect yourself and others. These are:
1. Avoid crowded places. People over the age of 60, and those with serious chronic medical conditions should avoid going to places where there are many people. This means avoiding movie theaters, crowded shopping centers, air travel, public transportation, and the church. If your workplace involves traveling or being with many people, ask about telecommutingz, if possible.
2. Wash your hands. We cannot emphasize this enough. Wet your hands with clean, running water, then rinse with soap. Rub both sides, between your fingers, and under your nails for at least 20 seconds. Be thorough and follow the technique recommended by the WHO.
3. Use hand sanitizers when you cannot wash your hands. When soap and water are not one option, use a hand sanitizer that contains at least 60% alcohol. Keep a bottle in the car, on your desk and in your purse or pocket.
4. Disinfect surfaces regularly. Clean high-contact surfaces like countertops, light switches, door knobs and the interior of your car with disinfectant. Use a mixture of 60% isopropyl alcohol and 40% water to kill germs on high-contact objects and surfaces, such as your cell phone, computer keyboard, remote control, door knobs and water taps. Wash the glasses with soap and warm water every day.
5. Cover your mouth and nose when you cough. Discard all used tissues immediately.
6. Give up handshakes and hugs for the moment. Practice greeting with a smile and putting your hands to your heart.
7. Do not wear a mask. Standard surgical face masks do not serve as a filter against the virus in healthy people, but if you are sick, a mask can help prevent droplets from spreading when you sneeze or cough, so it will not infect other people. The Sanitary Authorities have asked the healthy people not to accumulate masks because the priority is that health care providers have them since there could be a shortage if the general public buys them.
8. Call as soon as possible. If you have cold or flu symptoms, call your doctor to the toll-free numbers authorized for this purpose by the different Autonomous Communities instead of rushing to receive urgent care. Do not go to the hospital or medical center without first informing the health personnel, because you could infect other people.
9. Stay up-to-date by consulting reliable sources. Check back regularly for updates, and follow the mainstream media and health authorities, such as WHO and the Ministry of Health, Consumer Affairs and Social Welfare.
10. Stay at home


















Leave a Reply